Pulmonary Haemorrhage
Pulmonary Haemorrhage
Dec 03, 2025
Pulmonary Haemorrhage
Pulmonary haemorrhage is not uncommon in paediatric respiratory practice and can present with a wide spectrum of severity. Early recognition is essential, as identifying the precise source of bleeding — whether airway, lung parenchyma, or extrapulmonary — is crucial for guiding accurate diagnosis and management. Prompt, targeted intervention improves outcomes and helps prevent recurrence or complications.

Introduction
- Pulmonary haemorrhage is a condition which results in the extravasation of blood into the lung airways, parenchyma or alveoli.
- It can either be from the bronchial circulation or the pulmonary circulation and can either be focal or diffuse bleeding.
- The cause of focal pulmonary haemorrhage is usually from the airways and is frequently from the bronchial circulation and spares the alveoli.
- Diffuse alveolar haemorrhage (DAH) occurs when there is bleeding as a result of injury to the pulmonary capillaries, venules or arterioles.
- DAH leads to blood filling the alveolar spaces and can rapidly compromise gas exchange.
- This chapter focuses on diffuse alveolar haemorrhage in children.
Table 1: Causes of Haemoptysis
| Focal haemorrhage | Diffuse alveolar haemorrhage |
|---|---|
|
Immune mediated:
Non-immune mediated:
|
Table 2: Mimics of Haemoptysis
| Mimics |
|---|
|
Clinical Presentation
Diagnosis
- Classic triad of haemoptysis, chest infiltrates and anaemia.
- In children, haemoptysis may be absent and present as cough.
- Usually normocytic, normochromic anaemia; if chronic, may be microcytic hypochromic.
History
- Recurrent respiratory symptoms; may or may not report haemoptysis.
- Treated for anaemia but not responding to therapy.
- Underlying clinical conditions:
- Connective tissue disease.
- Systemic lupus erythematosus (SLE).
- Renal disease.
- Infections including pulmonary tuberculosis.
- Congenital malformations.
- Cardiovascular disease.
- Bleeding disorder.
Clinical signs
- As above, with signs of underlying condition.
- Acute respiratory distress (if acute bleed).
- Tachypnoea.
Investigations
Blood
- Full blood count (FBC), reticulocyte count.
- Coagulation screen (INR, fibrinogen).
- Immunoglobulins (IgA, IgG, IgE).
- *Autoimmune screen:
- Rheumatoid factor.
- Anti-dsDNA (double stranded deoxyribonucleic acid).
- ANA (antinuclear antibody).
- p-ANCA (perinuclear anti-neutrophil cytoplasmic antibodies).
- c-ANCA (cytoplasmic anti-neutrophil cytoplasmic antibodies).
- Anti-ribonucleic acid antibodies.
- Factor VIII.
- Von Willebrand’s factor.
- Anti-GBM (glomerular basement membrane) antibodies.
- Anti-MPO (myeloperoxidase) antibodies.
- Anti-PR3 (proteinase 3) antibodies.
- Cow’s milk allergen IgE.
- Coeliac IgA transmutase.
- Urine dipstick.
Bronchoscopy
- Blood or blood-stained fluid; identification of cause of bleed (congenital malformations, lymph nodes, pulsatile masses, pulmonary tuberculosis lesions, etc.).
- Bronchoalveolar lavage: haemosiderin-laden macrophages, free iron.
Chest radiograph
- Findings depend on nature of bleed.
- Diffuse lung changes.
- Acute/massive bleed:
- Consolidation.
- “White out”.
- Chest infiltrates.
- Chronic disease:
- Chest infiltrates.
- Interstitial changes.
- Diffuse changes.
Chest CT scan
- Ground-glass appearance with mosaic attenuation.
- Fibrosis.
- Cysts.
Echocardiogram
- Presence of congenital heart disease, arteriovenous malformations, mitral valve disease.
- Presence of pulmonary hypertension.
Lung biopsy*
- Not mandatory but can guide management.
- Tests performed (see appendix)*.
- May show haemosiderin-laden macrophages, free iron, red blood cells, fibrosis, capillaritis with or without immunoglobulins, complement factors, micro-organisms.
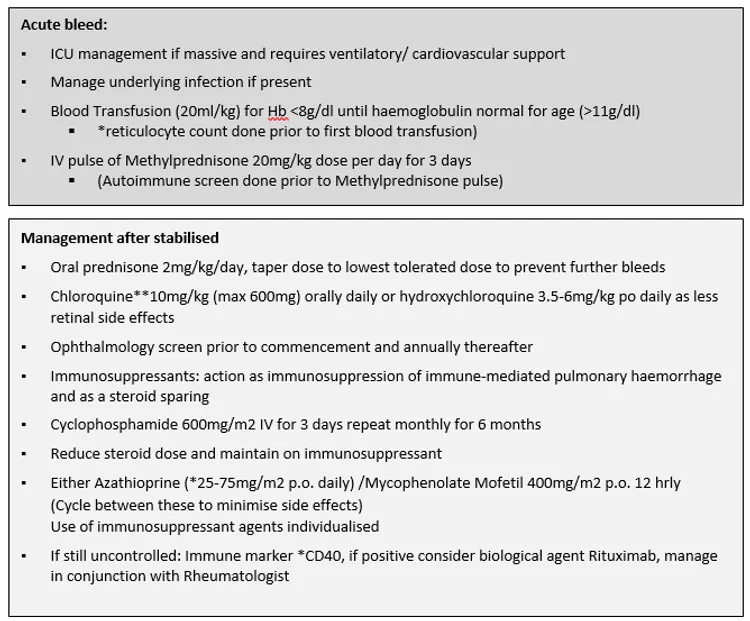
Figure 1: Management of Children with Diffuse Alveolar Haemorrhage
Follow-up
- Regular review as needed and until stable.
- FBC, reticulocyte count and chest radiograph at every visit.
- Lung function testing:
- Spirometry – in poor chronic control, restrictive pattern may be seen, although normal function is also frequent.
- DLCO (diffusing capacity of the lungs for carbon monoxide), as available.
- Active bleed:
- Drop in haemoglobin and increase in reticulocyte count with or without presence of respiratory symptoms.
- Changes in lung function tests consistent with acute bleed.
- Increase in DLCO
- Chest radiograph
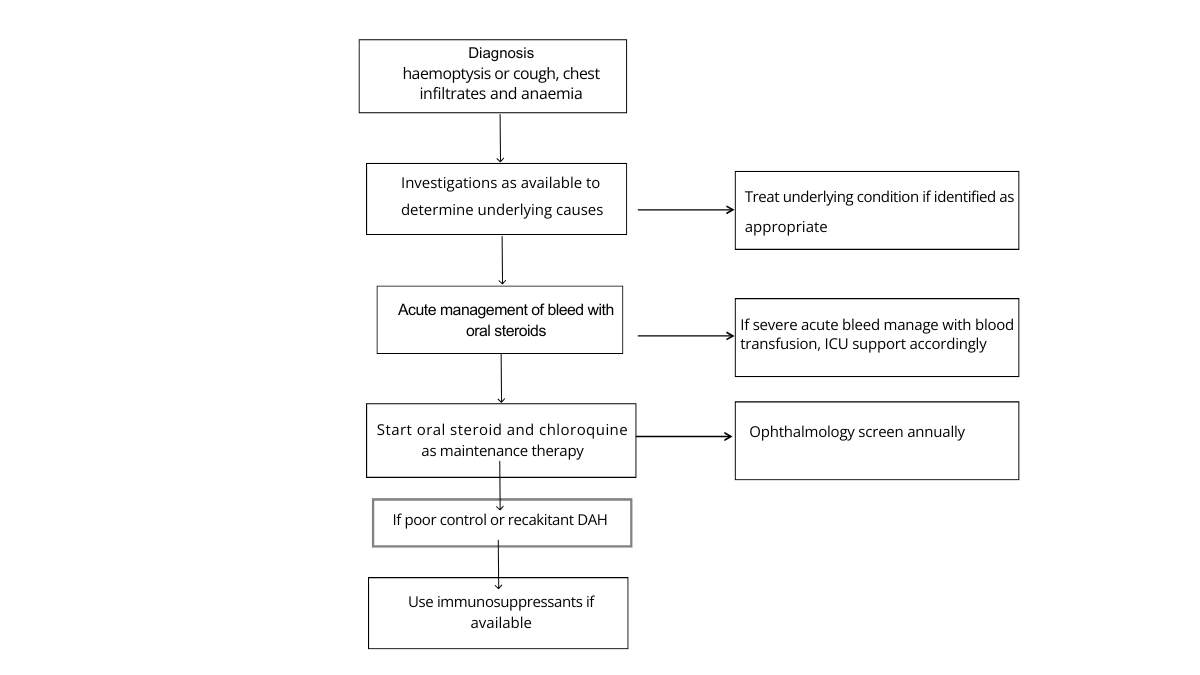
Fig 2: Algorithm for Management of DAH in a resource constrained setting.
Complications
- If repeated episodes:
- Pulmonary fibrosis.
- Respiratory failure.
- If acute massive bleed:
- Decompensation.
- Respiratory failure and cardiovascular collapse.
- Death.
Prognosis
- Varies between patients.
- Depends on underlying condition.
- Aim to use lowest dose of steroids necessary for control of disease.
- Bone-protective treatment:
- Calcium supplement and vitamin D (400 IU orally daily).
- Isoniazid prophylaxis* for those on certain immunosuppressants and biologicals.
References
- Godfrey S. Pulmonary hemorrhage/hemoptysis in children. Pediatr Pulmonol. 2004 Jun;37(6):476–84. doi: 10.1002/ppul.20020. PMID: 15114547.
- Avital A, Springer C, Godfrey S. Pulmonary haemorrhagic syndromes in children. Paediatr Respir Rev. 2000 Sep;1(3):266–73. doi: 10.1053/prrv.2000.0058. PMID: 12531089.
- Balfour-Lynn IM. Haemoptysis: is it really from the lungs? The well child who spits out blood. Arch Dis Child. 2023 Nov;108(11):879–883. doi: 10.1136/archdischild-2022-324276. Epub 2023 Mar 29. PMID: 36990647.