Paediatric Oscillometry
Paediatric Oscillometry
Paediatric oscillometry is an effort-independent lung function test that measures airway resistance and reactance during quiet breathing. It is particularly valuable for assessing young children or those unable to perform spirometry, and is sensitive to small airway abnormalities, bronchodilator response, and early disease changes.

1. What is Oscillometry?
Oscillometry is a non-invasive, effort-independent test that assesses airway resistance and reactance (inverse of compliance) by superimposing small pressure oscillations on normal tidal breathing. Unlike spirometry, it does not require forced exhalation, making it particularly suitable for young children, the elderly, or those unable to perform forced manoeuvres. It is able to detect airway obstruction, including small airway disease, and bronchodilator response.
2. What does Oscillometry Measure?
Oscillometry measures respiratory impedance (Zrs), which includes two components: resistance (Rrs), measuring airflow; and reactance (Xrs), measuring the stiffness of the airways and lungs. Throughout this chapter, simplified terms are used:
| Abbreviation | Measurement | What is Shows |
|---|---|---|
| R5 | Resistance at 5 Hz | Reflects total airway resistance (central + peripheral) |
| R20 | Resistance at 20 Hz | Primarily reflects central (large airway) resistance |
| R5–R20 | Difference between R5 and R20 | Indicates frequency-dependent resistance; increased values suggest small airway involvement |
| X5 | Reactance at 5 Hz | Reflects lung compliance and elastic recoil; more negative values indicate peripheral obstruction or reduced compliance |
| AX | Area under the reactance curve (below zero) | Cumulative measure of peripheral airway dysfunction; sensitive to early changes |
| Fres | Resonant frequency | Frequency where X5 = 0; elevated in severe obstruction and increased lung stiffness |
3. Indications for Paediatric Oscillometry
Indications are similar to those for spirometry (Chapter X). Oscillometry is particularly useful for detecting small airway disease, ventilation inhomogeneity, bronchodilator response. It is very useful in those too young or sick to do spirometry or other lung function tests.
| Category | Purpose |
|---|---|
| Diagnosis | Identify airway abnormalities in children who cannot reliably perform spirometry |
| Monitoring | Assess disease progression or response to treatment in conditions such as asthma, cystic fibrosis (CF), or bronchopulmonary dysplasia (BPD) |
| Screening | Evaluate lung function in high-risk groups, e.g., children born preterm or with a family history of asthma |
| Research | Collect lung function data in early childhood for longitudinal studies or population-based surveillance |
4. Contraindications to Paediatric Oscillometry
Respiratory oscillometry is a low-burden, passive test performed during quiet tidal breathing and is generally safe, including in young children and frail patients. No oscillometry-specific contraindications are defined in current ERS technical standards. General contraindications to lung function testing and local policies should still be followed. In routine paediatric practice, consider postponing the test if the child is:
- Distressed or uncooperative (crying, unable to sit calmly, or not tolerating the mouthpiece and nose clip)
- Acutely unwell with a respiratory infection (e.g. bronchiolitis, pneumonia, influenza) such that quiet, relaxed tidal breathing cannot be maintained
- Very full after a large meal in the last ~30 minutes, if this interferes with comfortable posture or relaxed breathing
- Recently given a bronchodilator, when baseline (pre-bronchodilator) values are required – unless a post-bronchodilator response is being assessed
Always document recent bronchodilator use (drug, dose and timing) and the reason for any deferred test.
5. Oscillometry Pre-test Preparation
Before testing, ensure the child is calm, seated upright with feet flat on the floor, and understands the simple breathing instructions. Avoid large meals, vigorous exercise, and short-acting bronchodilators in the period recommended by local policy and always record any recent medication use. Check that the nose clip fits comfortably, the mouthpiece seal is tight, and an adult is ready to gently support the child’s cheeks during the manoeuvre.
6. Performing Oscillometry in Children
Oscillometry is performed during quiet, tidal breathing and is generally well tolerated, even by children under six years of age. The child sits upright, wearing a nose clip, with cheeks supported while breathing through a mouthpiece and bacterial/viral filter. A minimum of three technically acceptable recordings of 20–30 seconds each should be obtained to ensure repeatability and reliability.
6.1 Key steps:
- Create a calm environment: Minimise noise and distractions; allow time for the child to settle.
- Explain the procedure simply: Use child-friendly language, e.g. “You’re just going to breathe like normal while the machine gently measures how your lungs are working.”
- Achieve a tight seal: Ensure the child’s lips are wrapped firmly around the mouthpiece with no air leaks.
- Apply a nose clip: The child must breathe only through the mouthpiece; the nose clip helps prevent air escape through the nose.
- Maintain good posture: Seat the child upright, feet supported, with the head in a neutral, forward-facing position.
- Stabilise cheeks and jaw: Firmly support the cheeks and lower jaw throughout the test to reduce upper airway shunting and minimise artefact.
- Encourage quiet, steady breathing: Ask the child to stay still, breathe normally and avoid talking, laughing, humming, or sighing during the measurement.
- Monitor real-time traces: Observe the on-screen flow, volume and pressure/impedance traces for artefacts such as coughing, swallowing, leaks, irregular breathing or breath holds and repeat any affected recordings.
6.2 Tips for Successful Testing
- Use age-appropriate distractions: Short videos, picture books or simple toys can help the child remain calm and still without changing their breathing pattern.
- Offer a practice run: Let the child try a brief “practice breath” before recording to build familiarity and confidence.
- Give frequent praise: Use encouragement and small rewards to reinforce good cooperation and make the experience positive for the child and family.
7. Evaluating Oscillometry Data Quality
High-quality, reproducible measurements are essential for valid clinical interpretation and for comparing results over time.
7.1 Acceptability Criteria (Single Acquisition)
An individual recording is acceptable when:
- Breathing is quiet and regular throughout the measurement (typically 16–30 seconds, depending on age).
- Flow–time and volume–time traces are stable, without sudden pauses or spikes.
- No artefacts are present, including cough, glottic closure, swallowing, speech, laughing, breath holds, tongue blocking the mouthpiece, or visible leaks around the mouth.
- After removing artefactual breaths (if breath-by-breath editing is used), at least three artefact-free breaths remain in the acquisition.
7.2 Repeatability Criteria (Between Acquisitions)
Between measurements, repeatability is considered acceptable when:
- At least three technically acceptable acquisitions have been obtained in the same session.
- The within-session coefficient of variation (CoV) for resistance at the lowest frequency (e.g. R5) across accepted trials is:
- ≤ 15% in children
- ≤ 10% in adults where applicable.
- R–f and X–f curves (especially X5 and AX) show similar shape and magnitude across accepted trials on visual inspection, supporting reproducibility.
These criteria should be applied alongside any additional, device-specific quality indicators provided by the manufacturer.
8. Interpreting the Oscillometry Test Result
8.1 Normal Ranges
| Parameter | Normal Z-score range | Interpretation when abnormal |
|---|---|---|
| R5, R20 | −1.64 to +1.64 | Z > +1.64 indicates increased airway resistance. |
| X5 | ≥ −1.64 | Z < −1.64 suggests reduced compliance and/or peripheral airway obstruction. |
| AX | No universal standard | Elevated values reflect cumulative reactance abnormality and peripheral airway dysfunction. |
| Fres | No universal standard | Higher values may indicate stiffer lungs and/or more severe obstruction. |
Note: Z-scores between −1.64 and +1.64 are generally considered within normal limits (5th–95th percentile).
In summary:
- R5, R20, AX and Fres values above the upper limit of normal (ULN; typically Z > +1.64) are abnormal.
- X5 values below the lower limit of normal (LLN; typically Z < −1.64) are abnormal/low and suggest disease.
- The further a result lies beyond the LLN or ULN, the greater the likelihood that it represents true disease rather than normal variation.
- All results must be interpreted together with the pre-test probability of disease, other clinical information and the quality of the test.
8.2 Recognising Oscillometric Patterns
Oscillometry can help distinguish between central and peripheral airway involvement by analysing how resistance and reactance behave at different frequencies.
| Pattern | Typical findings | Clinical interpretation |
|---|---|---|
| Normal |
|
No evidence of obstruction. |
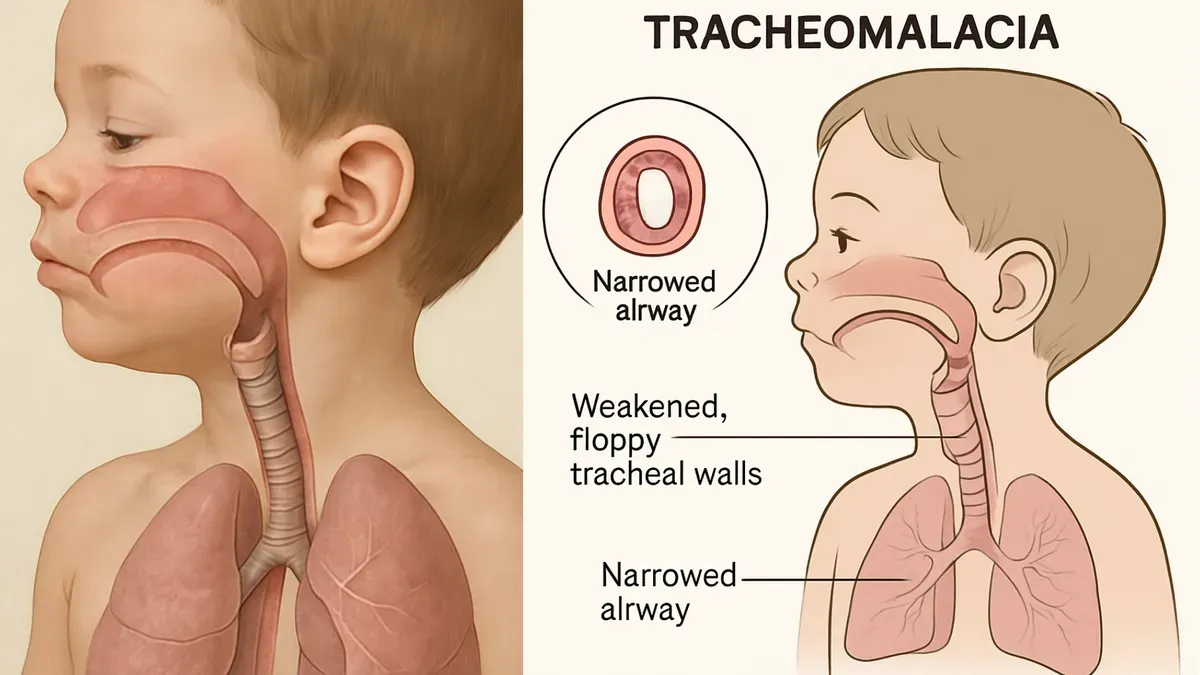
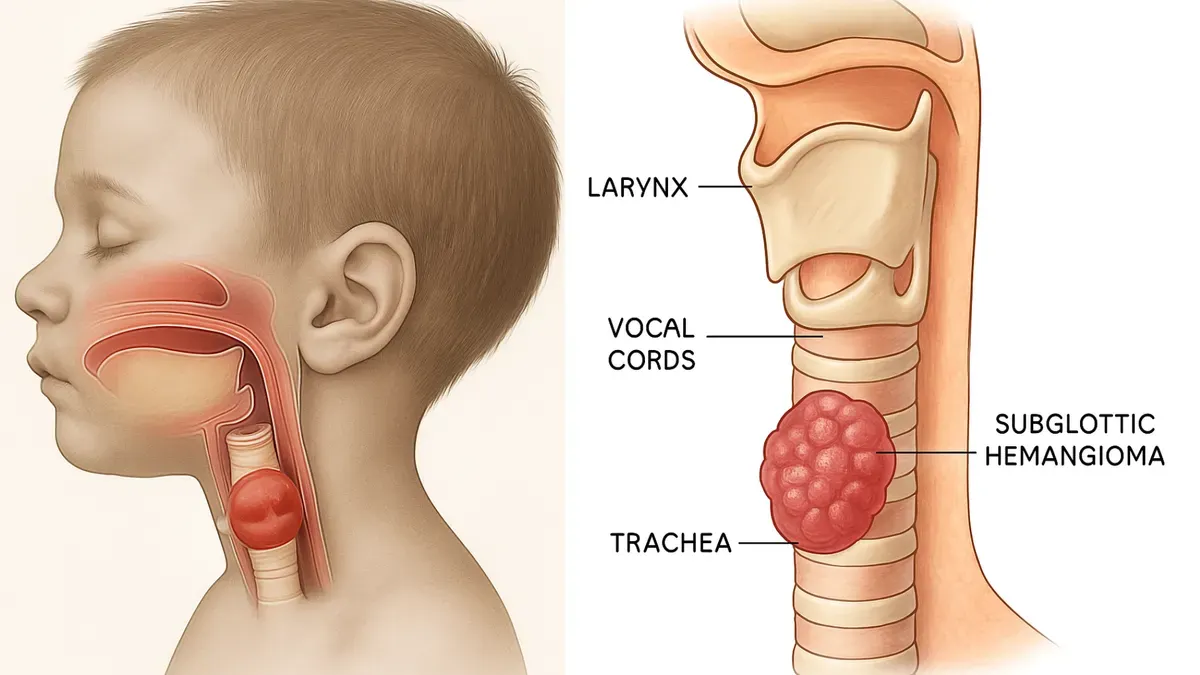
| Central obstruction |
|
Large airway involvement (e.g. tracheal stenosis). |
| Peripheral obstruction |
|
Small airway disease (e.g. asthma, bronchiolitis). |
| Mixed obstruction |
|
Combined central and peripheral airway obstruction (e.g. asthma). |
Interpretation tips:
- R5 reflects total airway resistance.
- R20 reflects central/large airway resistance.
- R5–R20, X5 and AX are particularly sensitive to peripheral airway involvement.
- Always correlate findings with clinical presentation, pre-test probability, test quality, and other investigations.
8.3 Assessing Bronchodilator Response (BDR)
Definition
Bronchodilator response (BDR) on oscillometry is a clinically meaningful improvement in airway mechanics following administration of a standard dose of a short-acting bronchodilator (e.g. salbutamol), compared with baseline (pre-bronchodilator) measurements.
In practice, this is usually reflected by consistent changes in several parameters, for example:
- Decrease in R5 (and often R5–R20)
- Decrease in AX
- Decrease in Fres
- Less negative X5 (movement towards normal)
Some laboratories use specific percentage change thresholds (e.g. a marked fall in R5 and/or AX) to define a definite BDR. Exact cut-offs vary, and you should follow your local SOP and reference values.
Important paediatric considerations
- Evidence for rigid BDR thresholds in children is still evolving.
- Children often have smaller absolute changes than adults, especially if baseline obstruction is mild.
- Smaller but consistent improvements across parameters (for example, a modest fall in R5 and AX with X5 moving towards normal) may still represent a clinically significant BDR in a child when:
- test quality is good, and
- the changes fit with the clinical picture (e.g. typical asthma symptoms, improvement after bronchodilator).
Therefore:
- Do not rely on a single numeric threshold alone.
- Look for a pattern of improvement across parameters.
- Always interpret BDR in the context of symptoms, pre-test probability, baseline obstruction, test quality, and day-to-day variability.
References
- King GG, Bates JHT, Berger KI, Calverley P, de Melo PL, Dellaca RL, et al. Technical standards for respiratory oscillometry. Eur Respir J. 2020;55(2):1900753. doi:10.1183/13993003.00753-2019
- Oostveen E, MacLeod D, Lorino H, Farre R, Hantos Z, Desager K, et al. The forced oscillation technique in clinical practice: methodology, recommendations and future developments. Eur Respir J. 2003;22(6):1026–1041. doi:10.1183/09031936.03.00089403
- Global Lung Function Initiative (GLI). Airway Oscillometry Reference Equations [Internet]. Available from: https://www.gliairwayosc.org